Message from the Chair


Dr. Richard G. Ellenbogen, Professor and Chair, Neurological Surgery
2020 was an immensely challenging and unique year. That is an understatement! I think some of the adversity we faced is captured in this current edition of the Montlake Cut. We witnessed a team of faculty, administrative staff, residents, scientists, nurses and students (in no particular order) demonstrate their resilience, perseverance and ability to adapt or outmaneuver any obstacle. Every day it was a new issue, and every day there was another novel solution that put a smile on my face. When Plan A did not work, the Neurological Surgery team adopted Plan B through Z. You can see that resilience and honesty in the research articles written by our residents on the effect of COVID on our practice and patients, and in the celebration of a new professorship for Dr. Kim. There is surprisingly little complaining about our fate and not surprisingly, much humor, tireless work and courage, as many of our folks were forward facing, in terms of the risk! It was certainly difficult and depressing at times, but with this newsletter edition you will see a team sustained by dedication to our mission and each other. We rose together in 2020, albeit we mourn those friends, family and patients who were less fortunate or did not survive. We are all thankful to work in the UW Department of Neurological Surgery as we reimagine a better future in 2021.
Special Announcement

The Kim family: Aylin, Louis, Azalea (11), Kenan (7), and Ziya (3). Credit: Louis Kim
Louis J. Kim, MD, MBA named Wallace T. Staatz Endowed Professor in Neurological Surgery
Time for celebration! Louis J. Kim has been appointed on January 1, 2021 to the Wallace T. Staatz Endowed Professorship in Neurological Surgery. This endowment was originally purposed by the generous Mr. Staatz to "enhance the University's ability to attract and retain distinguished faculty in neurological surgery”. Selected candidates for the Wallace T. Staatz Endowed Professorship in Neurological Surgery, as defined in the endowment agreement, “shall have demonstrated, through professional activities, expertise in neurological surgery”.
Well, there is no better choice for the Staatz professorship than Louis J. Kim, MD, MBA (LJK). When Dr. Kim was graduating from his residency and fellowship, his mentor, the renowned neurological surgeon Dr. Spetzler, Chair at the Barrow Neurological Institute, discussed his confident prediction of Louis. He assured me, as I was recruiting him, that he will be an academic superstar within a decade. Louis arrived at UW in 2007 and within 9 short years he had risen to Professor and Chief of Neurological Surgery at Harborview Medical Center, and subsequently Vice Chair of the department. He exceeded everyone’s expectations of him.
I will pick only 5 things, out of a multitude of achievements I can rattle off the top of my head, that LJK has accomplished at UW Medicine that are remarkable, deserving of his new endowment.
1) LJK started the Stroke and Applied Neuroscience Center at UW (SANS) based on Louis’ and Mike Levitt’s individual R0-1 NIH grants. The SANS goal is to discover ways to understand, treat and prevent stroke, cerebrovascular disease and other neurological disorders through research, education and outreach. Louis created this while running a busy practice, growing his laboratory, teaching residents and fellows and earning his MBA degree from the Foster School of business.
2) LJK ran the QI/QA safety arm of Neurological Surgery. He developed such an impressive patient safety system that the American Board of Neurological Surgery (ABNS) adopted his QI template.
3) LJK became Chief of Neurological Surgery at HMC and helped exponentially grow the neurological surgery service clinically, academically and educationally to one of the busiest and highest acuity ones in the nation.
4) LJK built the neurological surgery endovascular service (Levitt/Kim) in concert with an unparalleled open microsurgical/vascular/skull base team (Sekhar/Ferreira). He helped create a truly unique service that grew national/international reputation because it offered a diverse spectrum services to very complex surgical problems.
5) As a result of 4) he was able to convince the HMC leadership to build a Hybrid/Biplane OR suite at HMC (see article), build a CAST approved endovascular fellowship, become a regularly requested examiner off the ABNS and trained the first UW neurologist, Dr. Melanie Walker, who is now busily performing neuro-endovascular surgery at UW Medicine.
Congratulations Professor Louis J. Kim, MD, MBA. We are proud to be your partner!
Contributed by Rich Ellenbogen, MD
Patient Care

Harborview Medical Center’s Hybrid Bi-Plane Operating Room Credit: University of Washington Harborview Medical Center
UW Harborview Medical Center Hybrid Bi-Plane OR wins National Award from the Design-Build Institute of America
Congratulations to the design-build team responsible for Harborview Medical Center’s (HMC) new Hybrid Bi-Plane OR, whose work has been awarded the Design-Build Institute of America’s 2020 National Award for Best Small Project, Healthcare Facilities. This award showcases not only an extraordinary project, but also how the project team went above and beyond, achieving cost, schedule and quality goals, as well as demonstrating unique applications of design-build best practices. The envy of all our neurological surgeons, OR 6 in the main OR at HMC is unique and impressive. It has been a smashing success, large enough to house the Cerebrovascular/Endovascular surgical team and cutting edge enough to take on the most challenging patient conditions.
Hybrid bi-plane operating rooms are surgical suites that provide real-time patient imaging data, in this case a C-shaped biplanar imaging system that generates images on two separate planes, allowing a quick shift from diagnosis to surgical treatment in the same room. Hybrid operating rooms are sized and configured to exacting specifications. The rooms must support cardio- and neuro-medical teams, among others, and approximately 15,000 pounds of equipment. Physician teams, led by Chief of Neurological Surgery’s Dr. Louis Kim, communicated precisely the operating room functionality needed by the team and why. This highly technical surgical suite at HMC is one of only a handful of such facilities nationwide. Read more about the HMC hybrid OR project.
Research and Innovation
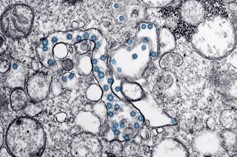
Transmission electron microscope image of an isolate from the first US case of COVID-19. Viral particles in blue, viral genome as black dots. Credit: CDC Newsroom Image Library
Considerations for Performing Emergent Neurointerventional Procedures in a COVID-19 Environment
Published in the journal Neurosurgery, UW Medicine faculty Louis Kim, Michael Levitt and members of the Endovascular Neurosurgery Research Group (ENRG) outlined practices to consider when managing COVID-19 patients requiring neurointerventional care. Recommendations cover the full course of care, from general planning, personnel, and facility considerations to preoperative, operative and postoperative best practices and are directed toward preventing exposure to other patients and healthcare personnel. Read the article.

University of Washington nursing students administer COVID-19 vaccines to UW Northwest staff. Credit: University of Washington
Economic Impact of COVID-19 on a High-Volume Academic Neurosurgical Practice
In a first report of its type, University of Washington Neurological Surgery residents Sanan Sivakanthan and James Pan, and faculty Louis Kim, Rich Ellenbogen, and Rajiv Saigal described the financial impact of COVID-19 on neurosurgery productivity and revenue. Using billing data from UW Medical Center and Harborview Medical Center, and comparing pre-COVID-19 (Jan 1-Mar 15, 2020) with post-COVID-19 (Mar 16-May 31, 2020) weekly average daily work relative value units (wRVUs), the authors document a decrease in wRVU as high as 76%, with a mean weekly loss of 51% initially. It was a “profound detrimental effect on surgical productivity and revenue generation” during the very beginning of the pandemic. Fortunately, this challenge was not sustained. The authors also shine light on the complexities associated with modeling economic impacts during this pandemic, a setting which necessitates novel and extremely rapid changes in how health care is delivered, and requires integration of simultaneous, ongoing, and dramatic social and economic challenges. Read the article.
Education

Training with ROSA. Credit: University of Washington Neurological Surgery
Early Effects of COVID-19 Pandemic on Neurosurgical Training in the United States: A Case Volume Analysis of 8 Programs
Newly arrived endovascular fellow Zaid Aljuboori worked with resident physician Chris Young, previous fellow Ryan Kellogg, scientific writer Sharon Durfy and faculty Mike Levitt and Rich Ellenbogen to research and document the effect of the COVID-19 pandemic on residency training programs across the United States. Their research compiled data on operative case volumes for 8 US neurosurgical residency training programs in early 2020. They found that March 2020 case volume was decreased by 15% compared with March 2019, but April 2020 case volume decreased almost 50% year-to-year. Their report also documented that all residency programs surveyed moved to providing didactics using online approaches, with 50% of respondents reporting the online format was improved compared to in person. Further, 87.5% of residency programs indicated that the COVID-19 pandemic resulted in increased time for research-related activity, with 62.5% of programs reporting an increase in the number of articles, abstracts or book chapters produced. The authors argue for the importance of ongoing data collection better to understand and address the impact of COVID-19 on residency training. Read the article.

I. Josh Abecassis, MD, training with the Home Microsurgery Lab (HML). Credit: Josh Abecassis
Developing microsurgical milestones for psychomotor skills in neurological surgery residents as an adjunct to operative training: the home microsurgery laboratory
Two superb Neurological Surgery resident physicians, Josh Abecassis (now an endovascular fellow at University of Miami) and Rajeev Sen, motivated by the decrease in operative and laboratory training opportunities due to the COVID-19 pandemic, looked for ways to continue to develop their microsurgical psychomotor skills. With guidance from senior authors Laligam Sekhar and Rich Ellenbogen, they designed and implemented a series of exercises, utilizing a metered stepwise approach, as part of a novel “home microsurgery lab” (HML). Techniques included dissection of turkey leg brachial artery and vein, end-to-end, side-to-end and side-to-side anastomosis using turkey brachial artery or silastic tubing, as well as the U-drill. In addition to developing the HML (for a cost of about $850), the authors outline a specific training program that addresses ACGME educational milestones and supports development of surgical competency, beginning with psychomotor proficiency developed by practice from home base. Read the article.
Residents News
Grants Received
Using Automated Pupillometry for Prediction of Intracranial Hypertension in Severe Traumatic Brain Injury
Richard H. Adler Attorney at Law & Adler Giersch Law Firm Endowed Fund for Traumatic Brain Injury Research, $5000

Congratulations to Guilherme Barros, MD, Madeline Greil, MD and Sananthan Sivakanthan, MD whose proposals have been selected for NIH funding effective July 1, 2021.
The goal of Dr. Barros' research under the mentorship of Drs. Kim and Levitt, is to understand how changes in hemodynamic flow after flow diverting stent (FDS) placement affect the aneurysmal endothelial cell transcriptional profile, ultimately determining a connection to treatment outcomes.
Working with Drs. Chesnut, Temkin and Bonow, Dr. Greil will perform research dedicated to identifying, through noninvasive means, patients with severe TBI who have intracranial hypertension.
Dr. Sivakanthan will work with Dr. Hofstetter on research directed toward developing animal models to assess intraspinal pressure in spinal chord injury and that can be translated directly to patient care.
Presentations
Home Microsurgery Lab. Microsurgery Training During the Covid-19 Pandemic
Talk at the American Association of Neurological Surgeons/Congress of Neurological Surgeons, Section on Pediatric Neurosurgery, December 2020

Implementation of the Patient Protection and Affordable Care Act (PPACA) Affects Treatment Modality in Sinonasal Squamous Cell Carcinoma
Talk at the North American Skull Base Society Annual Meeting, February 2021
People
Grants Received
Noninvasive tracking of intracranial pressure to improve care of traumatic brain injury
Garvey Institute for Brain Health Sciences Innovation Grant; $89,000
Viral reactivation from ganglia in subarachnoid hemorrhage
National Institutes of Neurological Disorders and Stroke, National Institutes of Health, $77,570
Discovery Omics for Targeted Treatment for Orphan Brain Cancers
Wayne D. Kuni and Joan E. Kuni Foundation, $1,200,000
Translating Single Cell Analysis into Actionable Therapeutic Strategies for Glioblastoma
Wayne D. Kuni and Joan E. Kuni Foundation, $900,000
Hemodynamic basis for secondary cervical grey matter tissue loss after spinal cord injury
National Institutes of Health, $1,957,000
Awards

Franck Kalume, PhD, included in Cell Mentor's List of 1000 Inspiring Black Scientists in America
New Team Members
Endovascular Fellow, Acting Instructor
Dr. Aljuboori joins Neurological Surgery from the University of Louisville, where he completed his neurosurgery residency. He has a particular interest in hemorrhagic and ischemic cerebrovascular disorders, including research on the effects of the fibrinolytic system on clinical outcomes.
Postdoctoral Scholar, Cerebrovascular Research Fellow
Dr. Shenoy completed medical school in Thane India, then traveled to Japan to complete a cerebrovascular research fellowship in Sendai, before joining UW Neurological Surgery. His research interests include topics at the intersection of clinical neuroscience and technology.

Newest members of the UW Neurological Surgery Family
On February 15, Dr. Rajiv Saigal and his wife Susy welcomed twins Dragan and Indira. Baby Boy Dragan came first, 7 lbs 15oz (left); Baby girl Indira arrived about 15 minutes later, 7 lbs 1 oz (right). Welcome to Draga and Indira and congratulations to Susy and Rajiv!




























