Overview
Brain surgery is used to verify a brain tumor diagnosis, decrease the effects caused by the pressure of the tumor mass within the skull and safely remove as much of the tumor as possible. Surgical tools include intra-operative CT scanning, stereotactic biopsy frames that were developed by a UW Medicine physician, brain mapping and 3-D frameless navigational systems.
For those patients requiring radiation, there is the gamma knife, LINAC and proton beam therapy.
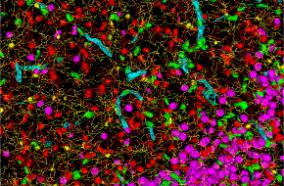
UW Medicine providers use the latest technology to diagnose and treat tumors of the nervous system. High-resolution MRI scanning of the peripheral nervous system, developed here, is capable of identifying tumors that other MRI scanners miss.
Every type of tumor is treated within the UW Medicine system of care, including gliomas, astrocytomas, glioblastomas, meningiomas, acoustic neuromas, schwannomas, pituitary adenomas, chondromas, medulloblastomas, ependymomas and esthesioneuroblastomas.
Procedural Details
For most patients, an MRI scan is administered the day they arrive for surgery. An intra-operative ultrasound is used in conjunction with the operating microscope and the MRI-based intra-operative navigation system to look at the brain.
From the MRI scanner, the patient is transferred to the pre-operative area, where an IV is administered by operating room nurses and anesthesiologists. From there, the patient is taken into the operating room.
The patient is then placed under anesthesia. Motor mapping and sensory mapping can be performed with the patient under general anesthesia. Some mapping, such as language mapping, requires the patient to be awake during the procedure. In such cases, the patient is kept under anesthesia except during the mapping part of the procedure. The Functional Brain Mapping article has more information.
Considerations
Brain tumors usually require surgery. This may be a biopsy to obtain a definitive diagnosis, or a larger operation to remove the tumor.
The surgical treatment of epilepsy is undertaken to remove the area of the brain where seizures begin. Tumor patients cared for by UW Medicine are evaluated by a multi-disciplinary team of specialists.
Each patient’s case is reviewed by the team at our weekly neuro-oncology tumor board meetings in order to determine the best treatment plan for each patient.
Effectiveness
The prognosis for brain tumors depends on the type of tumor and grade of malignancy. For some tumors, surgery can cure the brain tumor. For others, it is part of a multi-step treatment program that requires additional therapies after surgery to address invading tumor cells.
For the most malignant brain tumors, surgery is the first step of an aggressive, multi-step treatment. Following epilepsy surgery, patients who are seizure-free can begin the process of stopping anticonvulsant medication six months after surgery. Patients who remain seizure-free at two years rarely have recurrent seizures.
Risks
Surgical risks will vary depending on the size, location and type of tumor. Advances in technology and diagnostic accuracy now enable surgeons to work precisely and with amazing efficiency and reliability.
Surgical incisions have been reduced to an absolute minimum. Smaller incisions, less tissue trauma and better surgical planning have significantly reduced the risks associated with brain surgery.