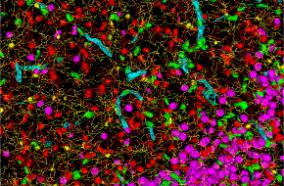
The goal of this project is to understand why a subset of GH-secreting PAs causing acromegaly do not respond well to surgical or medical therapies. Our central hypothesis is that low-allele frequency mutations within a tumor may reflect a driver cell population, resulting in a subset of aggressive PAs. We are requesting funding to test this hypothesis. We will develop a clinical-genotype and histological landscape from our large repository of tumor tissue from patients with GH-secreting PAs. We will identify somatic mutations and copy number variations at known oncogene hot spots, will evaluate the tumor transcriptome, and will correlate these findings with the extensive clinical data available in our repository. The ultimate goal is to be able to develop targeted treatments for treatment-resistant PAs.
Pituitary adenomas (PAs) are benign tumors of the pituitary gland, comprising approximately 15% of intracranial tumors. PAs are classified as functioning or non-functioning based on their ability to produce hormones. Although histologically benign, PAs may cause significant symptoms due to compression of adjacent structures or, in the case of functioning PAs, inappropriate hormone production. Poor outcomes are often caused by severe tumor-related endocrinological pathologies that persist despite maximal therapies. One example is acromegaly, which occurs with growth hormone (GH) secreting PAs. The goal of the proposed research is to investigate why a subset of GH-secreting PAs causing acromegaly do not respond well to surgical or medical therapies. We hypothesize that mosaicism and low-allele frequency mutations within these PAs may reflect a driver cell population, resulting in clinically aggressive PAs. We propose to develop a clinical-genotype and histological landscape from our large collection of GH-secreting PAs, to better understand the cellular pathways and clinical significance of mutations in these difficult-to-treat tumors. Acromegaly, with an annual incidence of 5 per 1 million people, is a disorder of GH hypersecretion causing disproportionate bone, soft tissue, and organ growth. Patients often have 10 years of active disease before diagnosis, and may suffer from arthritis, face and acral changes, glucose intolerance, and swelling of tongue, heart, kidney, and colon. If untreated, acromegaly results in cardiovascular, cerebrovascular, and pulmonary complications that overall are associated with a 30% shorter lifespan. Diagnosis requires elevated GH plus elevated insulin-like growth factor 1 (IGF-1), together indicative of chronic peripheral tissue exposure to elevated GH and correlated with clinical severity of acromegaly. Surgical resection remains the first line treatment in most patients with PAs and acromegaly, however, the rate of complete remission with surgery alone is only about 40%. Therefore, treatment of these tumors often consists of surgical resection, followed, if necessary, by one of several pharmacologic options. First line treatments include octreotide or lanreotide, somatostatin receptor ligands (SRLs). These treatments may fail due to different expression level of somatostatin receptors (SSTR) on the tumor surface in 30-70% of patients. After failing these, a second generation SRL or the GH receptor antagonist pegvisomant may be used. Current treatment strategies are largely based on a trial-and-error approach, and many patients continue to have difficulty achieving remission in the face of this challenging disease.