Overview
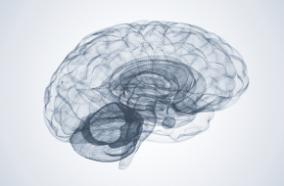
The UW Medicine Pituitary Program at Harborview offers state-of-the-art neuroradiology services to detect pituitary tumors.
Here are some of the studies your doctor may recommend:
-
Typically, diagnosis will begin with a magnetic resonance imaging (MRI) study. Our cutting-edge scanners (3T and 1.5T) — all equipped with the most up-to-date software — produce high-resolution images that allow doctors to better find and treat your tumor.
-
We can also do dynamic pituitary imaging where a contrast agent helps radiologists distinguish normal tissue from pituitary lesions. This technique is especially useful in identifying small tumors that may be difficult to discern in standard images.
-
High-resolution, 3-D MRI technology allows doctors to see even the smallest biologically active tumors, which are invisible in standard images.
-
A diagnosis of Cushing’s disease can be further clarified through a procedure called cavernous sinus and inferior petrosal sinus sampling (IPSS).
Procedural Details
Inferior petrosal sinus sampling (IPSS) may be necessary if your MRI does not show a tumor, which can often happen with Cushing’s disease.
In this procedure, an interventional radiologist will insert a thin tube called a cannula into your groin with a catheter. The catheter is placed into the vein that drains the pituitary gland. Your doctor can then detect the secretion of hormones from the pituitary gland, which allows him or her to locate the tumor without ever seeing it.
Considerations
IPSS may be necessary if your MRI does not show a tumor, which can often happen with Cushing’s disease.
Effectiveness
If your doctor suspects you have Cushing’s disease, IPSS can help distinguish a pituitary tumor from one in another part of your body.
Risks
The risk from IPSS is minimal. Very rarely, internal bleeding can occur in your groin. This is called a hematoma, and it typically gets better on its own.